Quick Links
3 easy steps to begin your URAC accreditation
Downloads
Case Management Accreditation Overview
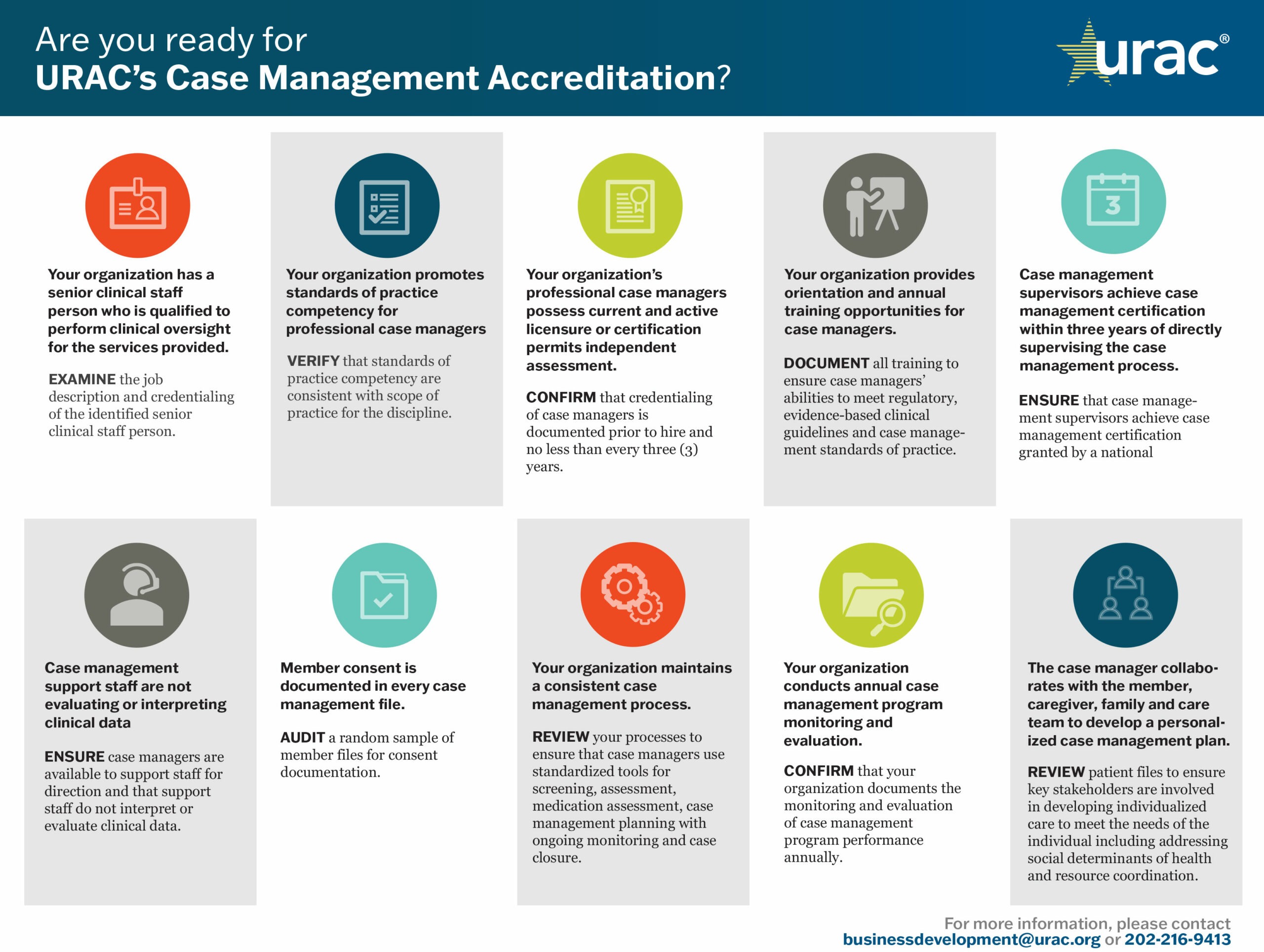
URAC’s Case Management Accreditation standards and performance measures address the increasing demand for excellence in care coordination, including improved patient engagement, service access and utilization and transitions of care. Understanding the intrinsic value of integrated care, URAC also includes behavioral health components into our case management standards.
URAC’s Case Management accreditation standards require companies to establish the policies, procedures and structure needed for optimal performance across four main principles of case management: care coordination, transitions of care, patient engagement and advocacy.
Health plans, payers, employers and government agencies recognize URAC Case Management Accreditation as a key catalyst in advancing collaborative care and patient advocacy, particularly for patients transitioning from inpatient care settings. Important to both private and public employers, URAC Case Management Accreditation also authenticates your Disability or Workers’ Compensation case management process to appropriately assess employee readiness for returning to work.
Once your organization begins the process, your organization can be fully accredited in six months or less.
Case Management Accreditation Benefits
By obtaining URAC accreditation, you distinguish your organizational leadership and accountability among other care management programs as well as your commitment to deliver high-quality coordinated care.
Benefits of Case Management Accreditation include:
- The ability to enhance patient satisfaction through an immersive experience that includes key stakeholders in patient care—consumers and their families, caregivers, providers and non-clinical staff
- Validation of your approach to improve health outcomes by predicting health-related behaviors, applying evidence-based, patient-centric goals and interventions and supporting self-care competencies
- Implementation of risk management oversight and review protocols that reduce client liabilities, enhance data security and ensure regulatory compliance
- Development of a blueprint for ongoing process and quality improvements that enhance care delivery and optimize operational efficiencies
Accreditation Process: What to Expect
At URAC, our accreditation process is more than collecting metrics and checking boxes. URAC offers your organization a collaborative, comprehensive learning experience designed to enhance knowledge and promote quality practices.
The program helps highlight the work your organization already does or can help guide your practice as you build the infrastructure to support case management.
Who May Apply
To be eligible for URAC’s Case Management Accreditation, an organization must provide interactive care coordination in collaboration with patients and other stakeholders. Organizations must be operating in the U.S. Download our Case Management Standards-at-a-Glance and Measures-at-a-Glance for more information.